Paper: "'I did not think they could help me':
UK-based autistic adults’ reasons for not seeking
public healthcare when experiencing suicidality"
This paper was published in 2025, in the journal Autism.
The two lead authors were Dr Tanya Procyshyn and myself (Dr Rachel Moseley). Our co-authors were Dr Sarah Marsden, Dr Carrie Allison, Dr Tracey Parsons, Dr Sarah Cassidy, Dr Mirabel Pelton, Dr Elizabeth Weir, Ms Tanatswa Chikaura, Ms Holly Hodges, Professor David Mosse, Dr Ian Hall, Dr Lewis Owens, Mr Jon Cheyette, Mr David Crichton, Professor Jacqui Rodgers, and Professor Simon Baron-Cohen (author links will open in separate tabs). The research was initiated, promoted and supported by charity Autism Action, whose number one priority is suicide prevention in autistic people.
You can click HERE to download a PDF of the paper. Please note that the full version of the paper may be triggering: it includes some distressing descriptions of suicidal thoughts and the experiences which led to them. Please take care of yourself; you may decide not to read it right now if you are in a vulnerable state.
Keep reading to see a plain English summary, or you can watch my explanatory video!
Why is this an important issue?
When people experience suicidal or mental health crises, public healthcare services like the UK's National Health Service (NHS) are, in theory, a source of help. We know that autistic people are much more likely than non-autistic people to struggle with their mental health and to experience suicidal thoughts. However, many autistic people in the UK do not seek NHS help when they experience suicidal thoughts.
While we know something about the barriers that autistic people can face when they try to access the NHS, we don't know enough about the reasons underpinning their decisions about whether or not to approach the NHS when experiencing suicidal thoughts. For example, do people avoid seeking NHS help because they do not want to be stopped from attempting suicide, or because they fear they will not be believed?
If we understand these reasons, we are better placed to tell policy-makers what needs to change in healthcare.
See below for a short video summary of this paper. You can open it up to large screen, and turn captions on and off by clicking the 'CC' button.
What was the purpose of this study, and what did the researchers do?
We wanted to understand the experiences of autistic adults in the UK when they sought NHS help for suicidal thoughts. In particular, we wanted to understand the reasons why autistic people did not seek NHS help. We also wanted to understand if these reasons differed by age and gender.
Working with the charity Autism Action and their advisory panel of autistic people and family members of autistic people, we designed an online survey, incorporating feedback from these advisors. It included questions about suicidal experiences; experiences of seeking help for suicidal thoughts (or reasons for not seeking help); experience of psychological therapies; app use; and ideas for preventing suicide. We published another paper using this data, which you can find here (link opens in new tab). In this paper, we focused on responses from autistic people who said they did not seek help from the NHS when they last experienced suicidal thoughts. Participants could select multiple pre-entered reasons for not seeking NHS help, as well as write in their own reasons. We looked at the reasons selected by participants, and analysed their free-text responses for themes (ideas) which cropped up across many participants.
What were the results of the study?
Of 1052 autistic adults from the UK, only just over a quarter (28%) sought help from the NHS when they last experienced suicidal thoughts.
We focused on the 72% who did not seek NHS help - their reasons for not seeking help (the pre-entered ones they could select from our survey) are shown to the right.
54% of our sample were autistic cisgender women; 25% were cisgender men, and 21% were transgender, gender-divergent, or gender-questioning. Almost 90% were white. All had some degree of experience with suicidal thoughts: 12% had had brief thoughts of suicide, 24% had had more prolonged suicidal thoughts, 30% had planned their own suicide, and 34% had attempted suicide at least once.
"I tried to cope and manage my feelings by myself" (58%)
The most commonly selected reasons for not seeking NHS help:
"The waiting list was too long - there was no point" (42.7%)
"I couldn't face trying to get a GP appointment" (34.1%)
"I did not think they could help me" (47.5%)
The least common reason for not seeking NHS help:
"I did not want to be stopped" (0%)
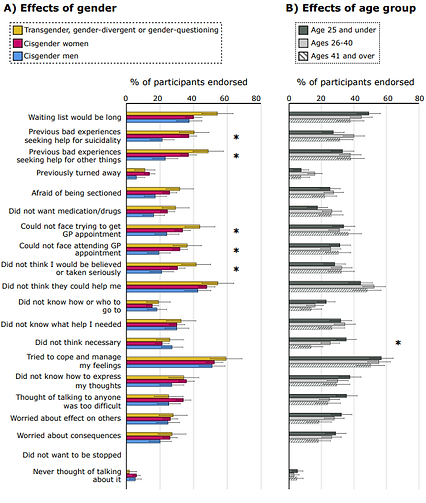
The bar charts below show selectable reasons for not seeking NHS help: reasons which were particularly likely to be selected by individuals of different gender identities are marked out with asterisks (*) on the left. reasons which were particularly likely to be selected by individuals of different age groups are marked out with asterisks (*) on the right.
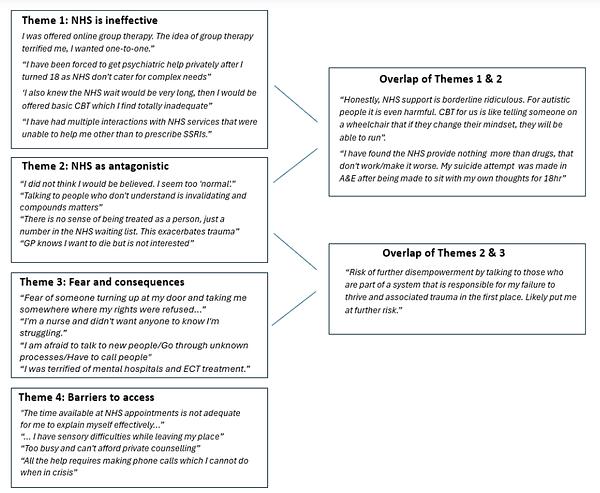
The image below shows the themes we identified in autistic people's self-written reasons for not seeking NHS help.
Autistic people's reasons for not seeking NHS help differed by their gender identity and age. You can see these differences in the figure to the left.
Compared to cisgender men, cisgender women and participants who were trans/gender-divergent were more likely to say they'd had previous bad experiences seeking help for suicidal thoughts or for other things, and to say they couldn't face attending the GP. Trans/gender-divergent participants, particularly, said they couldn't face trying to make an appointment with their GP, and worried they wouldn't be taken seriously.
Younger autistic people (those under age 25) were more likely to think that seeking NHS help was unnecessary.
We also looked to see whether reasons for not seeking help differed in relation to the extent of autistic people's experiences with suicidal thoughts and behaviour. People with experience of suicide attempts were more likely to say they'd had previous bad experiences seeking NHS help for suicidal thoughts and other things, that they had previously been turned away when they sought help, and to say they worried they wouldn't be believed.
Theme 1: "NHS is ineffective": autistic people often felt that the NHS did not have the specific skills or services to offer them; that the treatments on offer were ineffective or unhelpful for autistic people or 'complex' patients.
Theme 2: "NHS as antagonistic": autistic people often felt that encounters with the NHS had harmed their health and wellbeing. People often reported being misunderstood and invalidated by medical professionals, and did not trust the NHS.
Theme 3: "Fear and consequences": some autistic people worried about possible repercussions of help-seeking. These included experiencing stigma; having unwanted treatment forced upon them, or being sectioned; losing control; having information in their medical records which could affect their job, child custody, and other legal matters; or being denied gender-affirming healthcare
in future.
What are potential weaknesses in the study?
Our study was very specific to the UK, and our autistic participants were not representative of autistic people with learning disabilities and higher support needs, or autistic people of colour, who might face additional barriers to healthcare.
Our comparisons were a bit unbalanced, since we had more autistic women than men and trans/gender-divergent individuals. As such, our findings might not generalise to all autistic men, or to people with specific transgender or gender-divergent identities.
Very importantly, there are some autistic people who experience suicidality but choose not to participate in online surveys or to seek help - we don't know anything about these individuals, or how many autistic people die by suicide without ever having sought help.
Thank you for reading!
How will these findings help autistic adults now or in the future?
Our study confirms that autistic people often avoid seeking NHS help when they experience suicidal thoughts, and this is not because they don't want to be stopped.
Rather, our findings show that autistic people very much desire support, but have been let down by existing systems. Their responses are a wholly natural consequence of being hurt by and/or let down by the National Health Service.
This means that rather than trying to encourage autistic people towards health services that don't help (or even harm) them, the government needs to do more to ensure the NHS is capable of safely and appropriately supporting autistic people presenting with suicidal thoughts. There are some clear initial goals to start from, such as making GPs easier to access without needing to use the phone.
Our findings also show that autistic people of different genders and ages might have different reasons for not seeking help - and relatedly, have different needs in healthcare. Our findings suggest that more needs to be done to make healthcare safe and accessible for women and sex/gender minorities in particular - individuals who often are disbelieved when they seek help.
If you found this interesting, you may like to read:
If you are struggling with suicidal thoughts or your mental health, please look at the resources page in case there is something helpful there for you.